The untold origin story of the N95 mask April 27, 2020 – Posted in: In The News – Tags: Coronavirus Covid-19, Healthcare, Medicine, N95, Plague, Wu Lien Teh
The most important design object of our time was more than a century in the making.
Mark Wilson
It’s hard to think of a symbol of COVID-19 more fraught than the N95 respirator. The mask fits tightly around the face and is capable of filtering 95% of airborne particles, such as viruses, from the air, which other protective equipment (such as surgical masks) can’t do. It’s a life-saving device that is now in dangerously short supply. As such, it has come to represent the extreme challenges of the global response to COVID-19.
How did a flimsy polymer cup become the most significant health device of the 21st century? It all started in 1910 with a little-known doctor who wanted to save the world from one of the worst diseases ever known.
The first masks were about stopping smell
Going back even further—long before we understood that bacteria and viruses could float through the air and make us sick—people improvised masks to cover their faces, says Christos Lynteris. Lynteris is a senior lecturer at the Department of Social Anthropology at the University of St. Andrews, who is an expert in medical mask history.
He points to Renaissance-era paintings where people cover their noses with handkerchiefs to avoid illness. There are even paintings from Marseilles in 1720, which was the epicenter of the bubonic plague, that show gravediggers and people handling bodies with cloth around their faces, even though the plague was spread by the bites of fleas that traveled on rats.
“It was not meant to be against the contagion,” says Lynteris of the practice. “The reason these people were wearing cloth around their mouths and noses was, at the time, they generally believed diseases like the plague were miasma, or gases emanating from the ground. It wasn’t to protect you from another person, they believed plague was in the atmosphere—corrupt air.”
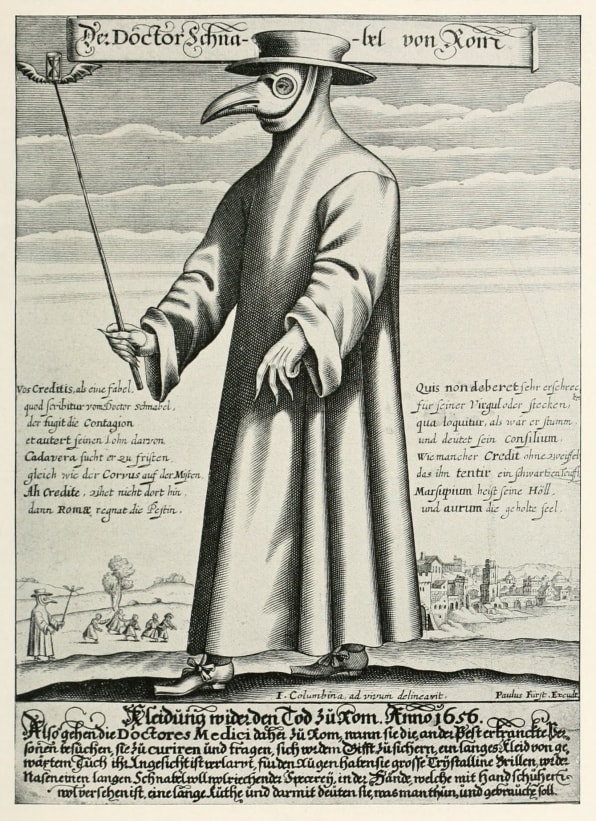
The theory of miasma is what drove the design of the infamous plague masks seen across Europe in the 1600s, which would be worn by doctors who identified the plague and marked the infected by tapping them with a stick. These elongated masks resembled large bird beaks and had two nostril ports at the edge of the mask that could be loaded with incense. People thought that by protecting themselves from the smell of the plague, they’d be protected from the plague itself.
“The stench causes disease. This [thought] continued all the way to the early 19th century,” says Lynteris. (It’s worth noting that, 200 years later, a French physician named Antoine Barthélemy Clot-Bey argued that the bird-like plague masks themselves were responsible for the spread of the plague because they made people scared, and a frightened body was at greater risk for disease.)
By the late 1870s, scientists learned about bacteria. Miasma fell from fashion as the modern field of microbiology emerged. And yet, what came next looked a whole lot like what came before—minus the creepy birds. “We often think of scientific paradigm shifts leading to breaks, but all the technologies used against germs by the end of the 19th century were [riffs] on technologies from miasma.”
A glorified handkerchief
Doctors started wearing the first surgical masks in 1897. They weren’t much more than a glorified handkerchief tied around one’s face, and they weren’t designed to filter airborne disease—that’s still not the point of surgical masks today. They were (and are) used to prevent doctors from coughing or sneezing droplets onto wounds during surgery.
This distinction between a mask and a respirator is important. It’s why healthcare professionals are upset that they’re being instructed to wear surgical masks when respirators are unavailable. Masks are not only made of different materials; they fit loosely on the face, so that particles can come in from the side. Respirators create an airtight seal so they actually filter inhalation.
The first modern respirator is born from plague—and racism

In the fall of 1910, a plague broke out across Manchuria—what we know now as Northern China—which was broken up in politically complex jurisdictions shared between China and Russia.
“It’s apocalyptic. Unbelievable. It kills 100% of those infected, no one survives. And it kills them within 24 to 48 hours of the first symptoms,” says Lynteris. “No one has come across something like this in modern times, and it is similar to the descriptions of Black Death.”
What followed was a scientific arms race, to deduce what was causing the plague and stop it. “Both Russia and China want to prove themselves worthy and scientific enough, because that would lead to a claim of sovereignty,” says Lynteris. “Whomever is scientific enough should be given control of this rich and important area.”
The Chinese Imperial Court brought in a doctor named Lien-teh Wu to head its efforts. He was born in Penang and studied medicine at Cambridge. Wu was young, and he spoke lousy Mandarin. In a plague that quickly attracted international attention and doctors from around the world, he was “completely unimportant,” according to Lynteris. But after conducting an autopsy on one of the victims, Wu determined that the plague was not spread by fleas, as many suspected, but through the air.
Expanding upon the surgery masks he’d seen in the West, Wu developed a hardier mask from gauze and cotton, which wrapped securely around one’s face and added several layers of cloth to filter inhalations. His invention was a breakthrough, but some doctors still doubted its efficacy.
“There’s a famous incident. He’s confronted by a famous old hand in the region, a French doctor [Gérald Mesny]… and Wu explains to the French doctor his theory that plague is pneumonic and airborne,” Lynteris says. “And the French guy humiliates him…and in very racist terms says, ‘What can we expect from a Chinaman?’ And to prove this point, [Mesny] goes and attends the sick in a plague hospital without wearing Wu’s mask, and he dies in two days with plague.”
Other doctors in the region quickly developed their own masks. “Some are…completely strange things,” Lynteris says. “Hoods with glasses, like diving masks.”
But Wu’s mask won out because in empirical testing, it protected users from bacteria. According to Lynteris, it was also a great design. It could be constructed by hand out of materials that were cheap and in ready supply. Between January and February of 1911, mask production ramped up to unknown numbers. Medical staff wore them, soldiers wore them, and some everyday people wore them, too. Not only did that help thwart the spread of the plague; the masks became a symbol of modern medical science looking an epidemic right in the eye.
Wu’s mask quickly became an icon through international newspaper reports. “The mask was a very novel thing…it had an effect of strangeness, which the press loved, but you imagine a black-and-white photograph with a white mask—it reads well,” says Lynteris. “It’s a marketing success.”

When the Spanish flu arrived in 1918, Wu’s mask was well-known among scientists and even much of the public. Companies around the globe increased production of similar masks to help abate the spread of flu.
The N95 is made for industries but arrives just in time to hospitals
The N95 mask is a descendant of Wu’s design. Through World War I and World War II, scientists invented air-filtering gas masks that wrapped around your entire head to clean the air supply. Similar masks, loaded with fiberglass filters, began to be used in the mining industry to prevent black lung.
“All the respirators were these giant, gas mask-looking things,” says Nikki McCullough, an occupational health and safety leader at 3M, which manufactures N95 respirators. “You’d wash them out at night and you could wear them again.”

This equipment saved lives, but it was burdensome, and a large reason why were the filters. The fiberglass required a lot of effort to breathe, and the full head enclosures were hot to wear. By the 1950s, scientists began to understand the dangers of inhaling asbestos, but people working with asbestos preferred not to wear bulky respirator masks. Imagine working in construction in 85-degree heat and having your head wrapped in rubber to protect yourself from an invisible threat.
Around the same time, a former décor editor for House Beautiful magazine named Sara Little Turnbull began consulting with the 3M’s giftwrap division. To make stiff ribbons, the company had developed a technology to take melted polymer and air-blast it into a fabric of tiny fibers. Turnbull realized a greater potential for this process, though, and she began experimenting with the material for shoulder pads, leveraging connections in the fashion industry for advice. Then in 1958, she gave a presentation at 3M simply titled: “Why,” which explained why 3M should go into this business of non-woven products in a bigger way. She presented over 100 product ideas for the technology, and was assigned to design a molded bra.
But the late ’50s were tough for Turnbull, who spent a lot of time visiting sick family members in hospitals. She lost three loved ones in quick succession. And out of that grief came a new invention: A “bubble” surgical mask that 3M released in 1961, that yes, takes its inspiration from the cup of a bra. When 3M learned it couldn’t block pathogens, the mask was re-branded as a “dust” mask.
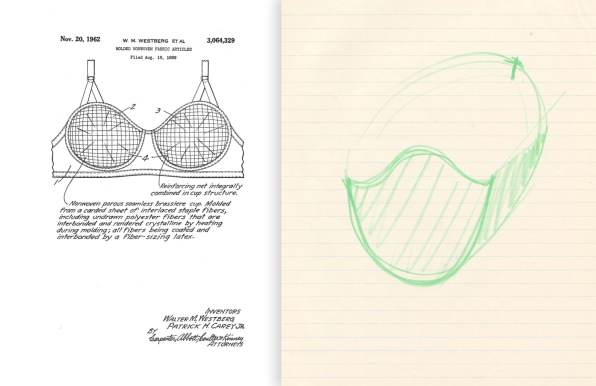
Of course, it was hard to build standards around something that didn’t even exist yet—for medicine or workplace safety. By the 1970s, the Bureau of Mines and the National Institute for Occupational Safety and Health teamed up on creating the first criteria for what they called “single use respirators.” The first single-use N95 “dust” respirator as we know it was developed by 3M, and approved on May 25, 1972. (Turnbull herself consulted on this line into the 1980s—and for many other corporate clients including General Mills, Ford, Corning, and Revlon.) Instead of fiberglass, the company repurposed that technology it had developed for making stiffer gift ribbons into a proper filter. Under a microscope, “they look like somebody dropped a bunch of sticks—and they have huge spaces between them,” says McCullough.
As particles, whether silica or viruses, fly into this maze of sticks, they get stuck making turns. 3M also added an electrostatic charge to the material, so even smaller particles find themselves pulled toward the fibers. Meanwhile, because there are so many big holes, breathing is easy.
The longer you wear an N95 respirator, the more efficient it becomes at filtering out particles. More particles just help filter more particles. But breathing becomes more difficult over time as those gaping holes between the fibers get clogged up with particles, which is why an N95 respirator can’t be worn for more than about eight hours at a time in a very dusty environment. It doesn’t stop filtering; it just prevents you from breathing comfortably.
N95 respirators were used in industrial applications for decades before the need for a respirator circled back to clinical settings in the 1990s with the rise of drug-resistant tuberculosis. HIV had a lot to do with its spread across immunocompromised patients, but tuberculosis infected many healthcare workers, too. To stop its airborne spread, N95 standards were updated for healthcare settings, and doctors began wearing them when helping tuberculosis patients. Even still, respirators are rarely used in hospitals to this day because it’s only outbreaks like COVID-19 that necessitate so much protection.
As Lynteris and many others point out, the respirator never really faded from significance in China. Wu went on to found China’s version of the CDC, narrowly miss winning a Nobel Prize, and be featured in many biographies (including his own autobiography). More recently, during the SARS outbreak, people in China wore facial protection to prevent the spread of illness. Then as pollution took over cities like Beijing, they wore respirators to filter pollution.
The N95 respirator isn’t perfect. It isn’t designed to seal well to the face of children or those with facial hair, and if it doesn’t seal, it doesn’t work as advertised. Furthermore, the N95 variants that are worn in high-risk operating rooms don’t have an exhalation valve, so they can get particularly hot to wear.
But the N95 respirator evolved over hundreds of years in response to multiple crises. That evolution will only continue through and beyond the COVID-19 pandemic. McCullough says that 3M is constantly reevaluating the N95 respirator, tweaking everything from its filters to its ergonomics. “My mom would say they look pretty much the same [as in 1972], but we want them to look simple so they’re easy and intuitive to use,” says McCullough. “We’re always improving the technology. We have thousands of scientists at 3M working on [it].”
This story has been updated to include the newly-unearthed contributions of Sara Little Turnbull.
About the author: Mark Wilson is a senior writer at Fast Company who has written about design, technology, and culture for almost 15 years. His work has appeared at Gizmodo, Kotaku, PopMech, PopSci, Esquire, American Photo and Lucky Peach.
This article first appeared on 24 March 2020 in Fast Company.
